Table of Contents
If you’ve ever sat in a doctor’s office or a therapist’s chair, you may have experienced the central diagnostic failure of modern healthcare. You describe the systemic causes of your distress—the crushing anxiety of navigating insurance claims, the sleepless nights over a bill you can’t pay, the hopelessness that comes from fighting a faceless bureaucracy. In return, you receive an individual diagnosis. You are treated as the casualty of a toxic system as if you were the cause of your own illness.
The cause of your suffering—a healthcare architecture where profit imperatives systematically override patient wellbeing—is the one thing that can’t be named.
This leaves us with a critical question: Why are the medical and psychological professionals who witness this suffering firsthand so silent? They are the experts on the front lines, the ones who see the emotional and physical wreckage every day. Why aren’t they sounding the alarm?
This article exposes the structural incentives that enforce this professional silence. This is not a story about individual cowardice but about a system that has become ruthlessly effective at protecting itself by muzzling the very people who have the authority to challenge it.
The View from the Trenches: Acknowledging Systemic Harm
Every day, medical and psychological professionals serve as silent witnesses to the devastating human cost of our healthcare system. They see the direct line between systemic policy and individual suffering. In clinics and hospitals across the country, they treat anxiety disorders directly tied to financial instability and depression linked to the hopelessness of fighting for basic care.
They see patients with chronic stress, burnout, and untreated conditions that fester until they become catastrophic, all because preventative care was inaccessible or unaffordable. They see early deaths that could have been prevented. They know, with absolute certainty, that the system is failing people on a massive scale.
This places them in an impossible position. They are tasked with treating the symptoms—the panic attacks, the chronic pain, the despair—of a sick system, while being professionally and institutionally forbidden from criticizing the disease itself. They are patching the wounds caused by a machine they are not allowed to say is broken.
The System’s Golden Handcuffs: Why Speaking Out is Dangerous
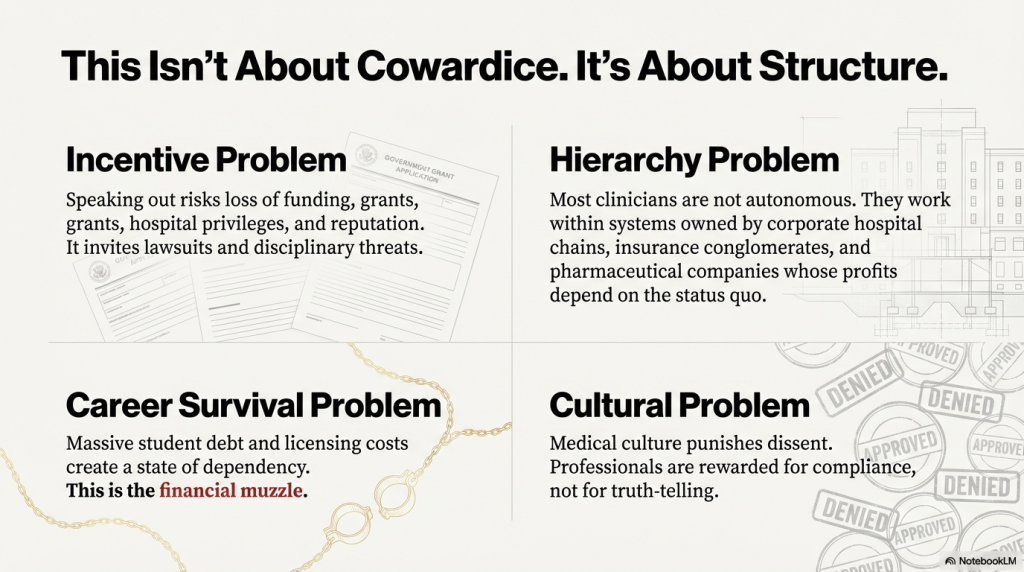
This widespread silence is not a sign of mass cowardice; it is the predictable outcome of a system designed to enforce it. The architecture of modern healthcare rewards compliance and punishes dissent through a series of powerful, interlocking incentives that make speaking out a career-threatening risk.
- The Funding Threat: Hospitals, universities, and research institutions depend on a steady flow of corporate and government funding to survive. A professional who speaks publicly about the systemic harms of the insurance industry or pharmaceutical pricing models risks being seen as a liability. This can lead to a direct loss of grants, research funding, and even hospital privileges, effectively cutting them off from the resources they need to do their work.
- The Hierarchy Trap: The romantic image of the autonomous doctor or independent therapist is largely a relic of the past. Today, most clinicians are not their own bosses; they are employees within massive systems owned by corporate hospital chains, insurance conglomerates, and private equity firms. Their jobs and career advancement are controlled by the very entities that profit most from the status quo. In this environment, criticizing the system is criticizing your employer.
- The Financial Muzzle: This hierarchy is reinforced by a crippling financial muzzle. The path to becoming a medical or psychological professional is paved with immense debt. The staggering costs of education, licensing, and malpractice insurance create a state of profound financial dependency that makes activism feel like an unaffordable luxury. When your family’s security depends on your paycheck, the risk of being fired or blacklisted for speaking out is simply too great.
- The Culture of Compliance: This financial dependency is further weaponized by a professional Culture of Compliance. From their earliest days of training, professionals are taught to follow protocols without question and to avoid making waves. Dissenters are often labeled as unprofessional, difficult, or disruptive. In a culture that values conformity over courage, survival depends on silence.
Psychology’s Great Paradox: Naming the Problem is Forbidden
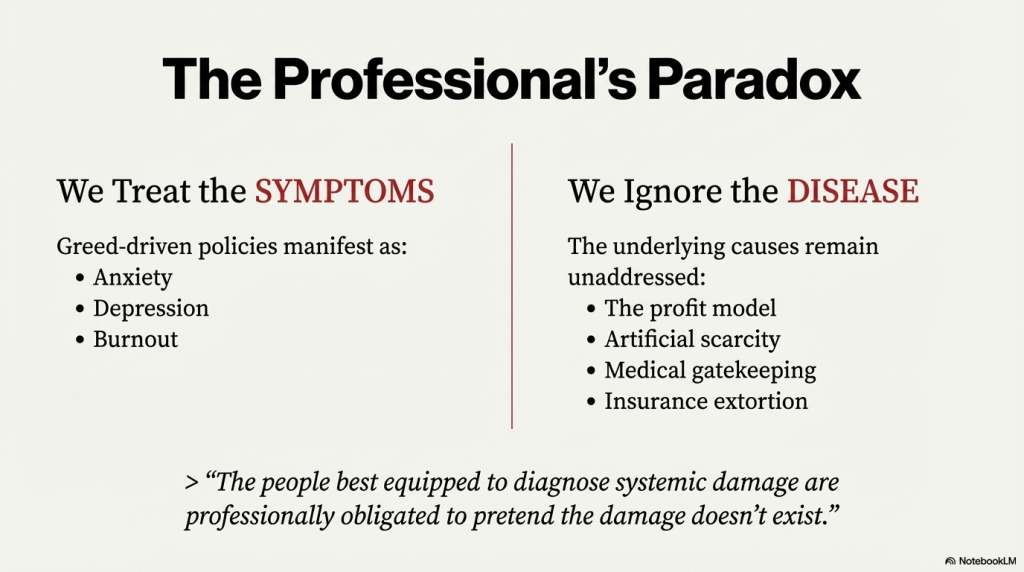
Nowhere is this conflict more acute than in the field of psychology. Therapists, counselors, and psychologists are uniquely trained to understand the systemic causes of distress—how poverty, discrimination, and economic instability create the conditions for mental illness. They know that a person’s anxiety is often a rational response to an irrational and threatening environment.
Yet, in practice, they are professionally obligated to treat this distress as an “individual pathology.” They must diagnose a person with an anxiety disorder, not with a justified fear of medical bankruptcy. They treat the symptoms caused by greed-driven policies but must ignore the disease: the profit model, the artificial scarcity of care, the medical gatekeeping, and the insurance extortion that define the patient experience.
This creates a profound paradox at the heart of the profession.
The people best equipped to diagnose systemic damage are professionally obligated to pretend the damage doesn’t exist.
When Silence Becomes Complicity
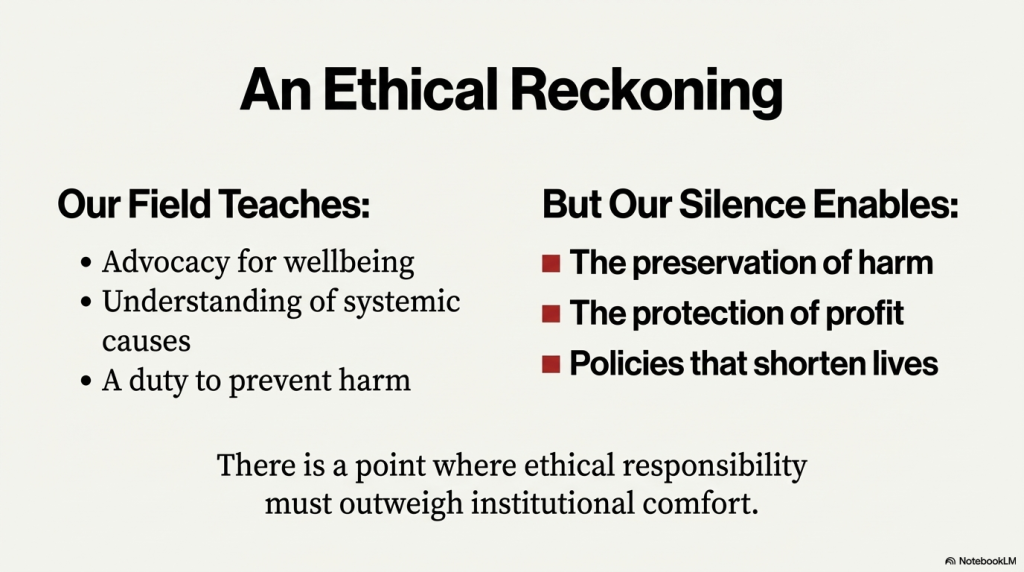
The stated ethical codes of both the medical and psychological fields are clear. They call on professionals to fulfill obligations of advocacy for wellbeing, understanding systemic causes, and preventing harm. But in a system that is actively and predictably causing widespread suffering, what does silence achieve?
Silence doesn’t challenge the policies that shorten lives. It preserves the profit motives that deny people care. It enables the very forces that are harming the people these professionals have vowed to serve.
In a collapsing and harmful system, silence is not a neutral act. It is a choice to protect institutional comfort over ethical responsibility. It is a decision to protect one’s own career at the expense of public wellbeing.
A Tipping Point for Truth
The need for experts to break this silence has never been more critical. The system is buckling under the weight of its own failures. Costs are becoming catastrophic for families, and people are dying from preventable and treatable illnesses. This is a psychological and medical crisis, inflicting moral injury on patients and providers alike.
Medical and psychological professionals hold a unique power that is desperately needed now. They have the authority to be heard and the credibility to break through public apathy. They have the access to see behind the curtain of the healthcare industry and can expose the real-world consequences of policies crafted in corporate boardrooms. If they do not speak out, the suffering will continue unchallenged, shrouded in a fog of political rhetoric and industry propaganda.
But a tipping point is coming, because the system’s failures are no longer abstract. It will arrive when a critical mass of professionals can no longer ignore the patients in front of them who have lost their insurance, lost their homes to medical debt, or lost loved ones to preventable conditions. At that point, the moral cost of silence may finally become unbearable. As the damage worsens, this silence is beginning to look like complicity.
Conclusion: A Moral Reckoning
Our healthcare system is not just broken; it is a toxic, profit-driven machine that has trapped its most knowledgeable professionals in a cycle of silence. This silence is not an accident—it is a feature, designed to protect the system from those who know its secrets best. And it is this silence that perpetuates immense and unnecessary human suffering.
There are no simple solutions. But the path forward begins with a moral choice, one that is facing every doctor, nurse, and therapist in the country. It is a choice that will ultimately define the integrity of their professions and the future of our collective wellbeing.
The question they must now answer—for themselves and for all of us—is the one that will determine what comes next.
“Do I stay silent inside a corrupt system, or do I defend the well-being of the people I vowed to serve?”
Here is an audio discussion I generated that offers some additional perspective on this topic.
Supporting Sources
- “International Comparison of Health Systems” — Kaiser Family Foundation (KFF)
Shows that the U.S. spends far more per person on health care than peer nations, yet does not get commensurately better outcomes. KFF+2Commonwealth Fund+2 - “The U.S. experiment with profit-driven health care has failed” — STAT News (2025)
Documents rising costs, healthcare-access problems, and how for-profit pressures are driving surging premiums and deteriorating care — underlining the systemic nature of the crisis. STAT - “Paying for It: How Health Care Costs and Medical Debt Are Making Americans Sicker and Poorer” — The Commonwealth Fund (2023)
Demonstrates that many insured Americans still struggle with medical debt and cost barriers, highlighting underinsurance and the failure of “coverage” to guarantee care. Commonwealth Fund
More articles about the culture of greed you might be interested in: